Start with the lowest effective dose. Your doctor will determine the appropriate starting point based on your specific condition and health history. This usually ranges from 2.5mg to 5mg daily, and adjustments are made based on your response to treatment.
Monitor for side effects closely. Common side effects include increased appetite, weight gain, mood changes, and insomnia. Report any concerning symptoms to your physician immediately. Early identification allows for timely intervention and potential dose adjustment.
Gradual tapering is key. Never abruptly stop prednisone. Your doctor will create a gradual tapering schedule, slowly reducing your dose over several weeks or months to minimize withdrawal symptoms and prevent potential health issues. This prevents the body from experiencing sudden hormonal shifts.
Consider potential drug interactions. Prednisone interacts with numerous medications. Provide your doctor with a complete list of all medications, supplements, and herbal remedies you take to avoid harmful interactions. This proactive step ensures safer and more effective treatment.
Regular check-ups are vital. Schedule regular appointments with your doctor for blood tests and other monitoring to assess your response to the treatment and make necessary adjustments to your medication plan. This ensures optimal therapeutic outcomes and early detection of any problems.
- Low Dose Regimen Prednisone: A Detailed Guide
- Understanding Low-Dose Prednisone: Dosage and Administration
- Common Administration Methods
- Dosage Adjustments
- Important Considerations
- Long-Term Use
- Common Uses for Low-Dose Prednisone: When is it Prescribed?
- Potential Side Effects of Low-Dose Prednisone: Monitoring for Adverse Reactions
- Gastrointestinal Effects
- Other Potential Side Effects
- Managing Low-Dose Prednisone Side Effects: Practical Tips and Strategies
- Long-Term Use of Low-Dose Prednisone: Considerations and Risks
- Tapering Off Prednisone: A Gradual and Safe Weaning Process
- Monitoring Your Body’s Response
- Managing Potential Side Effects
- Maintaining a Healthy Lifestyle
- Completing the Weaning Process
- Alternatives to Prednisone: Exploring Non-Steroidal Options
- Disease-Specific Approaches
- Lifestyle Changes
Low Dose Regimen Prednisone: A Detailed Guide
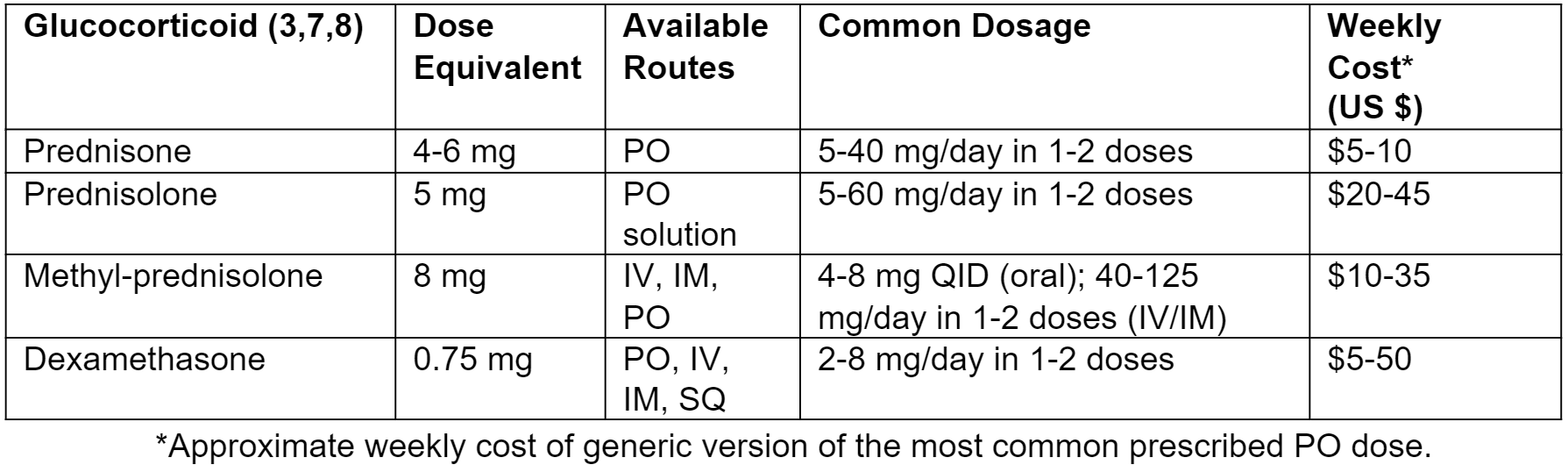
Consult your doctor before starting any prednisone regimen. Low-dose prednisone, typically 5-10mg daily, is often prescribed for inflammatory conditions like arthritis or allergies. This dosage aims to manage symptoms without significant side effects.
Remember, individual responses vary greatly. Your doctor will tailor the dosage and duration based on your specific needs and health history. Regular monitoring is vital to assess treatment efficacy and adjust the regimen as needed.
Common side effects at low doses may include mild insomnia, increased appetite, and mood changes. Higher doses increase the risk of more serious side effects like osteoporosis, cataracts, and increased blood sugar. Closely monitor yourself for any unusual symptoms.
Gradual tapering is crucial when stopping low-dose prednisone. Sudden cessation can cause adrenal insufficiency, a potentially serious condition. Your doctor will provide a safe tapering schedule tailored to your individual needs.
Here’s a table summarizing potential side effects and their management:
| Side Effect | Management |
|---|---|
| Insomnia | Maintain a regular sleep schedule, avoid caffeine before bed. |
| Increased Appetite | Choose healthy, balanced meals and snacks; monitor weight. |
| Mood Changes | Open communication with your doctor; consider stress management techniques. |
| Osteoporosis Risk (long-term use) | Discuss calcium and vitamin D supplementation with your doctor; weight-bearing exercise. |
| Elevated Blood Sugar (long-term use) | Regular blood sugar monitoring; discuss dietary adjustments and potential medication with your doctor. |
Maintaining open communication with your doctor is paramount. Report any new or worsening symptoms immediately. This ensures appropriate monitoring and adjustments to your treatment plan.
This information is for educational purposes only and does not constitute medical advice. Always seek professional medical advice before starting any medication.
Understanding Low-Dose Prednisone: Dosage and Administration
Low-dose prednisone typically ranges from 5 to 10 milligrams daily. Your doctor will determine the precise dosage based on your specific condition and health. Always follow your doctor’s instructions carefully.
Common Administration Methods
Prednisone is usually taken orally, as a tablet. It’s best to take it at the same time each day, often with food, to minimize stomach upset.
- Tablet Timing: Consistency is key. A regular schedule helps maintain consistent blood levels.
- Food Intake: Taking prednisone with food can reduce potential gastrointestinal side effects.
- Missed Dose: If you miss a dose, take it as soon as you remember, unless it’s almost time for your next dose. Never double up on doses.
Dosage Adjustments
Your doctor may adjust your dosage over time, depending on your response to treatment and any side effects. Regular monitoring of your condition and any potential side effects are crucial. Open communication with your doctor is vital throughout the treatment process.
Important Considerations
- Inform your doctor about all medications you are currently taking, including over-the-counter drugs and supplements, as interactions can occur.
- Report any side effects, no matter how minor they seem, to your doctor immediately. Common side effects may include increased appetite, weight gain, mood changes, and insomnia.
- Never stop taking prednisone abruptly without consulting your doctor. Stopping the medication suddenly can lead to withdrawal symptoms.
- Follow your doctor’s instructions for tapering off the medication. This usually involves gradually reducing your dose over a period of time to minimize withdrawal effects.
Long-Term Use
Long-term low-dose prednisone use requires careful monitoring for potential long-term side effects. Your doctor will conduct regular check-ups to assess your progress and manage any potential risks.
Common Uses for Low-Dose Prednisone: When is it Prescribed?
Low-dose prednisone (typically 5-10mg daily or less) finds application in various conditions. It’s frequently prescribed for:
- Autoimmune diseases: Managing symptoms of conditions like rheumatoid arthritis, lupus, and inflammatory bowel disease, often in conjunction with other medications. Low doses can help control inflammation and improve quality of life.
- Allergic reactions: Reducing swelling and inflammation from severe allergies, such as allergic rhinitis. It’s usually a short-term treatment to manage acute symptoms.
- Skin conditions: Treating inflammatory skin conditions such as eczema or psoriasis, often used as a short course to alleviate flare-ups.
- Asthma: Low-dose prednisone can help control severe asthma attacks or flare-ups when other medications aren’t sufficient. It’s typically used for short periods.
- Certain types of cancer: Used in combination with other cancer treatments in specific situations, but its use is highly dependent on the individual case and type of cancer.
Remember, prednisone is a powerful medication with potential side effects. A doctor will carefully consider your individual needs and health before prescribing it. They will determine the appropriate dose and duration of treatment based on your specific condition and response to the medication. Always follow your doctor’s instructions precisely. Regular monitoring may also be necessary.
Specific examples of prescription scenarios include:
- A patient with rheumatoid arthritis experiencing significant joint pain and swelling who is already taking disease-modifying antirheumatic drugs (DMARDs).
- An individual with a severe allergic reaction requiring rapid symptom reduction.
- A person with asthma experiencing a prolonged and serious attack despite using their regular inhalers.
This information is for general knowledge only and does not replace consultation with a healthcare professional. Always discuss your treatment options with your physician.
Potential Side Effects of Low-Dose Prednisone: Monitoring for Adverse Reactions
While low-dose prednisone generally causes fewer side effects than higher doses, monitoring for potential issues is crucial. Pay close attention to changes in your mood, including increased irritability or anxiety. Weight gain, often centered around the abdomen, is another common side effect. Keep track of your weight weekly to detect significant changes. Observe your blood pressure regularly, as prednisone can elevate it. Inform your doctor if you notice significant increases.
Gastrointestinal Effects
Upset stomach, heartburn, or increased risk of ulcers are possibilities. Report any persistent digestive discomfort promptly. Increased blood sugar levels are also possible, particularly if you have a predisposition to diabetes. Regular blood glucose monitoring is advised, especially if you have diabetes or risk factors. Increased risk of infection is another concern; note any signs of infection, such as fever, chills, or unusual fatigue. Lastly, be aware of potential for insomnia or sleep disturbances.
Other Potential Side Effects
Muscle weakness or thinning of the skin are less common but possible side effects. Report any unusual bruising or slow wound healing to your doctor. Regular check-ups with your physician are critical for monitoring your overall health while on low-dose prednisone. Open communication about any concerns ensures optimal management and minimizes potential risks.
Managing Low-Dose Prednisone Side Effects: Practical Tips and Strategies
Monitor your blood sugar regularly, especially if you have diabetes or a family history of it. Small increases in blood sugar are common with prednisone, even at low doses. Maintain a balanced diet and stick to your exercise routine to help manage this.
Stay hydrated. Drink plenty of water throughout the day to help prevent dehydration, a potential side effect. Carry a water bottle with you as a reminder.
Eat smaller, more frequent meals to avoid stomach upset. Prednisone can affect digestion. This approach can ease any discomfort.
Increase your calcium and vitamin D intake. Prednisone can weaken bones over time. Discuss supplementation options with your doctor. Consider foods rich in these nutrients, like dairy products and leafy greens.
Manage your blood pressure. Prednisone can elevate blood pressure. Check your blood pressure regularly and follow your doctor’s recommendations for medication or lifestyle changes.
Get enough sleep. Prednisone can disrupt sleep patterns for some individuals. Maintain a regular sleep schedule and create a relaxing bedtime routine to improve sleep quality.
Report any unusual symptoms to your doctor immediately. This includes but isn’t limited to: weight gain, mood changes, increased thirst, frequent urination, or vision problems.
Communicate openly with your doctor. Regular communication ensures they can adjust your treatment plan as needed, helping manage side effects and optimize your health.
Long-Term Use of Low-Dose Prednisone: Considerations and Risks
Low-dose prednisone, while offering significant benefits, presents potential long-term side effects. Doctors carefully weigh these risks against the treatment’s advantages before prescribing prolonged use. Regular monitoring is key.
Prolonged use, exceeding three months, increases the risk of osteoporosis. Bone density scans help track this risk. Calcium and Vitamin D supplementation, along with weight-bearing exercise, are often recommended.
Increased blood sugar levels (hyperglycemia) are another concern. Regular blood glucose monitoring is crucial, particularly for individuals with a predisposition to diabetes. Dietary adjustments and potentially medication changes may be needed.
Cataracts and glaucoma are possible ocular side effects. Regular eye exams allow for early detection and management of these complications. Treatment for these conditions might require collaboration with an ophthalmologist.
Weight gain is common. Maintaining a healthy diet and regular exercise help mitigate this. A nutritionist can provide personalized guidance on diet and lifestyle modifications.
Mood changes, including anxiety and depression, can occur. Open communication with your doctor is vital to address these concerns. They might suggest therapy or adjust medication.
Immunosuppression is a significant risk. This increases susceptibility to infections. Practicing good hygiene, avoiding crowds during flu season, and receiving recommended vaccinations are crucial preventative measures.
Withdrawal from prednisone should always be gradual, as sudden cessation can lead to adrenal insufficiency. Your doctor will create a tapering schedule to minimize this risk. This process needs careful medical supervision.
Regular check-ups allow for proactive management of potential side effects. Openly discuss any concerns with your physician to ensure optimal health and well-being while on low-dose prednisone.
Tapering Off Prednisone: A Gradual and Safe Weaning Process
Your doctor will create a personalized tapering schedule. Commonly, this involves reducing your prednisone dose by a small amount (e.g., 2.5-5mg) every few days or weeks. Never adjust your medication without consulting your physician.
Monitoring Your Body’s Response
Closely monitor yourself for withdrawal symptoms like fatigue, muscle weakness, joint pain, or nausea. Report any concerning changes to your doctor immediately. They might adjust your tapering schedule accordingly. Regular blood tests can help track your progress and ensure safe reduction.
Managing Potential Side Effects
Expect some side effects during the tapering process. Increased fatigue is common; prioritize rest and manage your activity levels. If joint pain arises, discuss pain management strategies with your physician. Dietary changes, including increased potassium intake, might help counteract some side effects.
Maintaining a Healthy Lifestyle
Maintain a balanced diet, ensure adequate hydration, and engage in moderate exercise as tolerated. Stress management techniques like meditation or yoga can be beneficial, particularly during the weaning period. Good sleep hygiene is also crucial for overall well-being and recovery.
Completing the Weaning Process
Once your doctor deems it safe, you’ll complete the tapering process. Continue monitoring for any lingering side effects. Follow-up appointments are important for assessing your progress and ensuring a complete recovery. Open communication with your doctor throughout the entire process is key.
Alternatives to Prednisone: Exploring Non-Steroidal Options
Consider non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen for pain and inflammation relief. These are widely available over-the-counter, but always follow dosage instructions carefully. Remember to discuss NSAID use with your doctor, especially if you have pre-existing conditions like kidney or liver problems.
Disease-Specific Approaches
Your treatment plan depends heavily on the underlying condition. For autoimmune diseases, biologics like adalimumab or infliximab can target specific immune system pathways. These medications require a prescription and close monitoring by your physician. Rheumatoid arthritis might benefit from disease-modifying antirheumatic drugs (DMARDs), such as methotrexate or sulfasalazine. These drugs modify the disease’s progression but may take time to show effects. Always discuss potential side effects with your doctor before starting any treatment.
Lifestyle Changes
Alongside medication, explore lifestyle adjustments. Regular exercise, a balanced diet rich in anti-inflammatory foods (like fruits and vegetables), and stress management techniques (such as yoga or meditation) may significantly improve symptoms and reduce reliance on medication. Maintain open communication with your healthcare provider to ensure your chosen alternatives are suitable for your specific needs and health profile.